Values-Based Interventions Increase Reenrollment and Equity among Community College Pre-Allied Health Students
Ross E. O'Hara*
Persistence Plus LLC
Betsy Sparrow
Persistence Plus LLC
Lois Joy
Jobs for the Future
Abstract
Addressing labor shortages within nursing and allied health professions, which have been exacerbated by the COVID-19 pandemic, requires increasing persistence and equity among community college students pursuing these fields. In this study, we adapted and combined three values-based interventions (values affirmation, goal congruence, and utility values) into one treatment, delivered via interactive text messages, with the goal to support reenrollment among pre-allied health students during the pandemic. Using institutional data from a statewide community college system, we randomized pre-allied health students who were enrolled in Fall 2019 and/or Spring 2020, and who had a valid mobile number on file, into treatment (n = 1,649) or control (n = 1,650) groups. Fully treated students received an average of 17 text messages over 8 weeks of Summer 2020; control students received business as usual support from the college. After adjusting for baseline differences in prior enrollment, the treatment significantly increased reenrollment by 3 percentage points (74% vs. 71%). Examination of individual differences revealed that effects were concentrated among men (+11 percentage points), Black/African American students (+7 percentage points), and students who were not enrolled in Spring 2020 (+13 percentage points). Values-based interventions, therefore, can be an important tool for addressing shortages and inequities in healthcare education and the labor force, an important step toward improving public health. Moreover, community colleges seeking to engage students who withdrew before or during the COVID-19 pandemic should leverage evidence-based practices to boost reenrollment.
Introduction
The COVID-19 pandemic has underscored the vital importance of skilled nurses and allied health professionals for the wellbeing of the United States. At the same time, the pandemic has exacerbated workforce gaps by simultaneously increasing demand and reducing supply of healthcare workers (Boyle, 2021). One solution is to boost student persistence within community college nursing and allied health programs, which have historically suffered from attrition rates as high as 47% and significant equity gaps in terms of gender, race, and ethnicity (Donini-Lenhoff & Brotherton, 2010; Harris et al., 2014; Pryjmachuk et al., 2009). These inequities not only limit the talent pool available to fill pressing vacancies, but also restrict people of color to the lower-skilled and lowest-paying roles in the healthcare system (Snyder et al., 2015). In our study, therefore, we developed and tested a novel combination of values-based interventions (Canning et al., 2018; Harackiewicz et al., 2014; Jordt et al., 2017) to increase retention and equity among community college students on the allied health track. Efforts such as this are necessary for increasing economic mobility of underserved populations, addressing labor force needs, and preserving public health.
Literature Review
Labor Shortages in Nursing and Allied Health
Concerns about healthcare workforce gaps in the United States predate the COVID-19 pandemic. By 2030, employment in health care occupations is expected to grow by 16%, or about 2.6 million new jobs (Bureau of Labor Statistics, 2021), during which time a sizable chunk of the healthcare workforce will reach retirement age (U.S. Department of Health and Human Services [DHHS], 2019). Given those trends, it has been estimated that several states will experience skilled workforce shortfalls of up to 40,000 nurses by 2030 (U.S. DHHS, 2017). Nursing homes are already stretched thin, as upwards of 15% reported shortages of nurses and nurse aides in May 2020, with average shortage rates exceeding 25% in some states (Xu et al., 2020). Schools also need nurses, as fewer than 40% employ a full-time nurse, and 25% have none at all (Willgerodt et al., 2018).
The COVID-19 pandemic, meanwhile, has increased anxiety symptoms, depressed mood, insomnia symptoms, and burnout among frontline healthcare professionals (Cai et al., 2020; Hu et al., 2020; Labrague & de los Santos, 2020; Said & El-Shafei, 2020), careers already marked by relatively high rates of burnout (Reith, 2018). For example, in April 2020, 57% of New York City healthcare workers screened positively for acute stress, 48% for depressive symptoms, 33% for anxiety symptoms, and 72% for insomnia symptoms (Abdalla et al., 2021; Shechter et al., 2020). Likewise, in a survey of United States healthcare workers collected from May to October 2020, 30% reported high levels of daily stress, 38% reported depression or anxiety, and 43% reported work overload (Prasad et al., 2021). These troubling trends deepen workforce gaps by driving away skilled professionals; job dissatisfaction and turnover intentions among nurses have increased during the pandemic, driven by stress, anxiety, and perceived threat or fear of coronavirus transmission (Falatah, 2021; Labrague & de los Santos, 2021).
Retention in Nursing and Allied Health Programs
Addressing both current and anticipated labor shortages in healthcare requires a robust talent pipeline, much of which in the United States is fed by community colleges (Bureau of Labor Statistics, 2019; Skillman et al., 2012). Unfortunately, the COVID-19 pandemic has wreaked havoc on overall community college enrollments, which are down nearly 15% since 2019, with the greatest losses observed among Black, Hispanic, Native Hawaiian or Pacific Islander, and American Indian or Alaska Native students (Howell et al., 2021; National Student Clearinghouse, 2021). Although data suggest that interest in nursing and healthcare is high, many community colleges cannot expand enrollments in these areas due to minimum thresholds for program entry (Chan et al., 2019) and/or limited resources such as faculty members and equipment (Weissman, 2021). To meet growing demand for nurses and allied health professionals, therefore, it is critical to maximize retention in these programs.
One way to increase retention is by improving equity. Although racial and ethnic diversity in these professions has steadily increased over the past two decades (Zangaro et al., 2018), people of color still tend to be concentrated within the lower-skilled and lowest-paying healthcare occupations (Snyder et al., 2015). Black and Latinx students also take longer to complete nursing and allied health programs, and are more likely to withdraw, than their White and Asian peers (Donini-Lenhoff & Brotherton, 2010; Pryjmachuk et al., 2009). Men are underrepresented, as well, constituting less than 10% of the nursing and nursing education workforce (Hodges et al., 2017). Along with a lack of role models and feelings of isolation in the profession, men face gender discrimination and challenges to their masculinity; reasons why they, too, take longer to complete programs and are more likely to withdraw compared to women (Pryjmachuk et al., 2009). Increasing equity in healthcare education, therefore, creates opportunities for men and people of color to start on and climb the healthcare occupational ladder and achieve better economic outcomes. Moreover, a diverse healthcare workforce holds the promise to reduce healthcare discrimination and foster better health among underrepresented populations (Phillips & Malone, 2014; Wilbur et al., 2020).
One way to retain a larger and more diverse pool of students in nursing and allied health programs is through increased and proactive student support. Insufficient support, including requiring students to self-identify a need for help and unresponsiveness when students do reach out, is a primary reason why nursing students withdraw (Chan et al., 2019). These barriers may be more impactful for men and students of color who are more likely to harbor doubts about whether they belong in college and/or healthcare, lack trusted advisors and/or role models, and experience both help-seeking threat and discrimination. In our study, therefore, we used an interactive text-messaging platform to provide proactive and responsive support to community college students in pre-allied health programs.
Adapting Values-Based Interventions for Pre-Allied Health
Content for these supportive text messages was adapted from three values-based interventions previously shown to improve performance, retention, and equity in science pathways (Diekman et al., 2017; Harackiewicz & Priniski, 2018). Although debate persists as to whether medicine, nursing, and allied health belong under the STEM (science, technology, engineering, and mathematics) umbrella, critics of their exclusion point to the array of STEM courses and skills necessary to graduate and succeed in these fields (Davidson, 2020; Green & John, 2020). Moreover, both STEM and nursing/allied health majors exhibit retention inequities based on gender, race, and ethnicity. We hypothesized, therefore, that values-based interventions could also benefit pre-allied health students.
These values-based interventions prompt students to reflect on their classroom experiences and future goals in order to shape their mindsets about an academic and professional field. First, values affirmation steels one's self-worth in the face of threatening environmental feedback, like a bad grade or a stereotype-driven negative experience, thereby preserving motivation and preventing withdrawal (Harackiewicz & Priniski, 2018). These brief writing exercises have improved performance in introductory biology and physics courses, especially among underrepresented students (Harackiewicz et al., 2015; Jordt et al., 2017; Miyake et al., 2010). Second, students opt out of science if they perceive their personal values as incongruent with those held by scientists (Diekman et al., 2017). Goal congruence interventions that combat erroneous stereotypes about who belongs in science have been shown to bolster students' intentions to continue in science (Brown et al., 2015; Diekman et al., 2011; Steinberg & Diekman, 2018). Finally, students are more likely to quit any program if they cannot see the practical relevance of the material. Utility value interventions encourage students to reflect on how they can leverage what they learn in class in their current, everyday lives, not just in some far-off career (Hulleman et al., 2017). Students who write about the relevance of their science courses report higher perceived value in learning science, earn better class grades, and exhibit stronger persistence in science pathways (Canning et al., 2018; Hulleman et al., 2010; Hulleman et al., 2017).
Our study expands upon earlier research in two important ways. First, we sought to extend the external validity of values-based interventions, which heretofore have been tested mostly within traditional science courses such as biology or physics (e.g., Canning et al., 2018; Jordt et al., 2017; Miyake et al., 2010). There is a dearth of knowledge, therefore, on whether these interventions can help students pursuing other STEM fields. We are the first, to our knowledge, to adapt these techniques to help pre-allied health students connect their personal values to their pursuit of healthcare credentials, reframe misconceptions about who belongs in allied health, and appreciate the everyday, practical utility of what they learn in class. Likewise, most studies have focused on baccalaureate-seeking undergraduates, with researchers only recently exploring whether and how values-based interventions work within community colleges (Canning et al., 2019; Tibbetts et al., 2018). Our treatment is designed specifically for community college students.
Second, most values-based interventions have been administered via classroom surveys and exercises, which require student attendance and class time. Text messaging, however, is an effective and scalable means for delivering interventions to, and modifying (or "nudging") behaviors of, college students (e.g., Loughran et al., 2018; Riley et al., 2008; Riordan et al., 2017). For example, text messages to help college-intending high school graduates fulfill matriculation requirements (e.g., registering for orientation, completing financial aid forms) increased fall enrollment rates by up to 7 percentage points (Castleman & Page, 2015; Page & Gehlbach, 2017). Moreover, text messages to help first-year community college students renew their financial aid increased persistence by at least 12 percentage points (Castleman & Page, 2016). Finally, a summer texting intervention that leveraged behavioral science in its message design increased fall reenrollment among community college STEM students by 10 percentage points (O'Hara & Sparrow, 2019). Our study leveraged an interactive text-messaging platform as a novel and scalable means for delivering values-based interventions.
Study Aims and Hypotheses
We designed an evidence-based treatment, delivered during Summer 2020 to community college students in a pre-allied health program, to promote reenrollment for Fall 2020. This treatment was highly relevant in light of the COVID-19 pandemic, which had limited students' access to their college campus and their typical support system, including faculty and advisors, and may have induced higher stress levels among this particular population interested in healthcare professions (Abdalla et al., 2021; Prasad et al., 2021; Shechter et al., 2020). We hypothesized that treated students would be more likely to reenroll for Fall 2020 than control students receiving business as usual support. Moreover, based on gender, racial, and ethnic inequities in nursing and allied health (Donini-Lenhoff & Brotherton, 2010; Pryjmachuk et al., 2009), as well as the tendency for values-based interventions to benefit those most at risk for withdrawal (e.g., Harackiewicz et al., 2015; Miyake et al., 2010), we hypothesized that both men and students of color would benefit from treatment more so than women and White students. Finally, we hypothesized that students who actively engaged with the treatment would be more likely to reenroll compared to treated students who did not engage (O'Hara & Sparrow, 2019).
Methods
Setting
Our study was conducted at Delaware Technical Community College (DTCC). DTCC is the sole community college in Delaware, and allied health1 is its largest program. Allied health, however, also has the highest average attrition rate of any DTCC major, reflecting the retention challenges historically faced by these programs (Harris et al., 2014). DTCC has four campuses throughout Delaware, but due to the COVID-19 pandemic, these campuses were closed during the study, the majority of summer instruction occurred online, and student support services (e.g., academic advising, tutoring) were consolidated to online and telephone formats. We did not customize treatment, stratify randomization, or analyze data with respect to students' "home" campus.
Participants
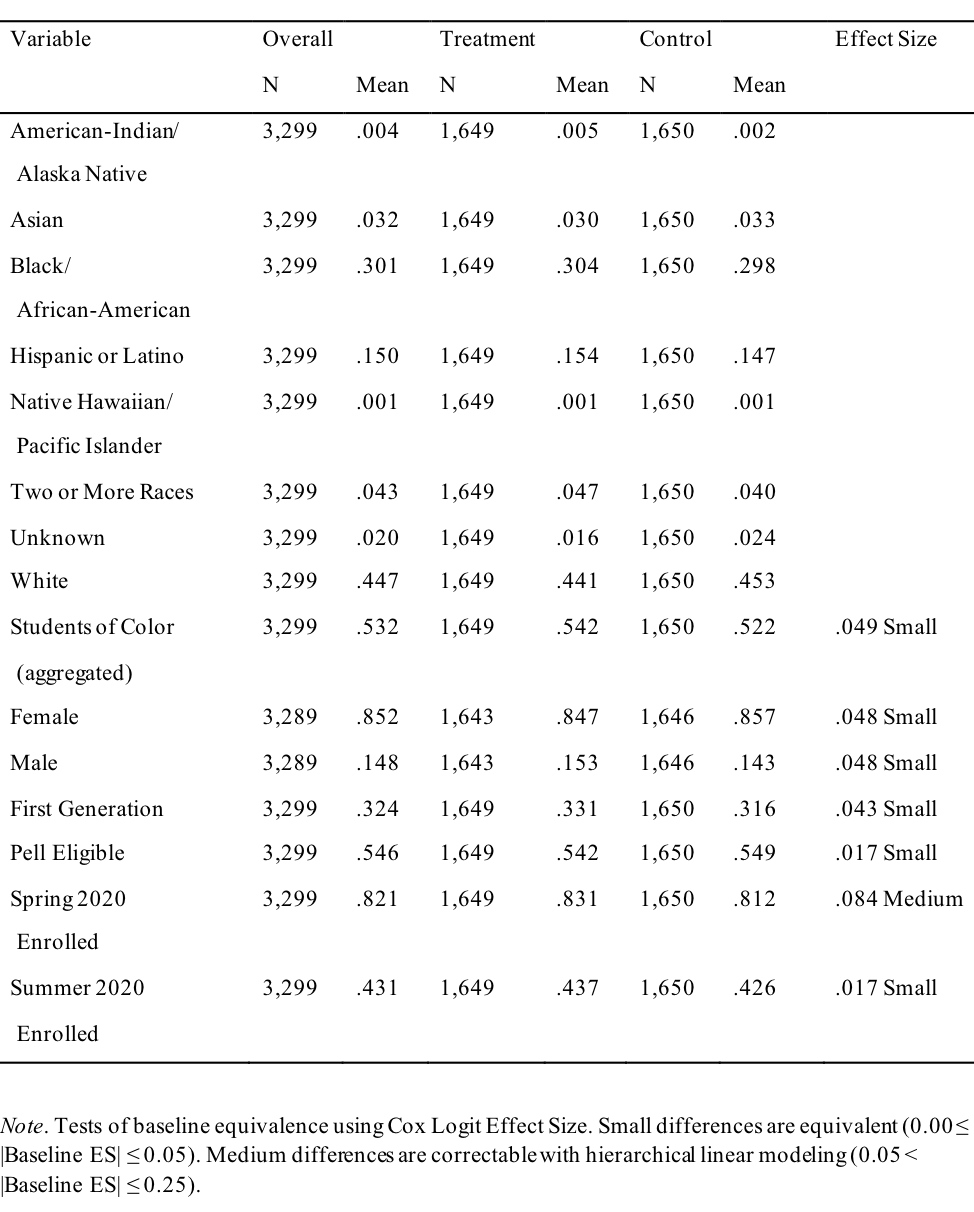
Students were eligible if they (a) attended DTCC in Fall 2019 and/or Spring 2020; and (b) had declared their intention to apply for the nursing or allied health program. These criteria produced 3,512 eligible students. We then removed 108 students (3.1%) who had a missing or invalid phone number (e.g., fewer than 10 digits), and used www.searchbug.com to identify and remove another 105 students (3.0%) whose phone numbers were disabled or a landline, leaving 3,299 students for randomization. We then randomly assigned 1,649 students to the treatment group and 1,650 students to the control group. As displayed in Table 1, 15% of students identified as male and 85% as female, and the majority identified as either White (45%), Black/African American (30%), or Hispanic/Latino (15%), with 53% of the population identified as students of color overall. Moreover, 32% of participants were identified as first-generation and 55% as eligible for the Pell grant. With regard to enrollment, 82% of students were enrolled in the semester immediately prior to treatment (Spring 2020), and 43% were enrolled during treatment (Summer 2020).
Table 1. Descriptive Statistics of the Sample: Overall and by Treatment Status with Baseline Equivalence
Procedure
Students in the treatment group were automatically enrolled into Persistence Plus, a proprietary service that delivers interactive text messages for educational purposes. Participants were informed about their right to opt out of receiving messages in an email sent before the study commenced, as well as within the first message. Students could opt out of messages at any time by replying with 'STOP' or 'UNSUBSCRIBE.' The sender of the messages was identified as 'myDTCC Support,' and messages were sent proactively on Tuesdays and Thursdays for 8 weeks of Summer 2020.
Messages were designed based on the previously described values-based interventions to encourage reenrollment at DTCC (see Appendix for examples). In addition, treatment participants received messages dependent on their enrollment status at the start of the study. For example, students who had yet to enroll for Fall 2020 were asked via text if they needed help with registration, financial aid, or career planning. A student who responded with 'financial aid' received contact information for DTCC's Office of Financial Aid & Scholarships, support for handling student loans, and advice regarding work-study options; students struggling with registration or career planning were given customized advice and directed to academic advising or career services, respectively. We collaborated with DTCC student advisors to personalize messages to the DTCC context, including phone numbers, websites, and appropriate vernacular. DTCC staff also identified student resources, such as the campus food pantry and CARES Act funds, that could be highlighted based on challenges students might express. This "local" scale up approach (Bird et al., 2021) balances personalization with cost and efficiency concerns, ensuring messages connect with students and avoid reactance that could be caused by a generalized, impersonal campaign.
Analysis
All variables were derived from official DTCC registrar data provided in June 2020 for student demographics and in October 2020 for academic outcomes. Following guidelines set out by the What Works Clearinghouse (2020), we first tested baseline differences between the treatment and control groups measured against standardized effect size in enrollment (0 = not enrolled, 1 = enrolled) for both the Spring 2020 and Summer 2020 terms, and for each of our baseline demographics, using Cox's Index for dichotomous variables:
As displayed in Table 1, randomization resulted in well-balanced groups with one exception: A greater percentage of Spring 2020 enrolled students were randomized into the treatment group (83%) compared to the control group (81%). Enrollment in the prior term is likely to have some impact on enrollment in the outcome term, Fall 2020. As this baseline difference was measured as a medium effect size (.08), appropriate statistical adjustment satisfied baseline equivalence (What Works Clearinghouse, 2020). Spring 2020 enrollment, therefore, was entered as a binary variable into hierarchical linear models when examining the impact of the treatment on Fall 2020 enrollment. In addition to this statistical adjustment, subsequent analyses show that the treatment worked primarily for students who were not enrolled in Spring 2020; thus, the direction of this baseline difference would likely attenuate the impact of our treatment.
The outcome of interest in this study was enrollment in Fall 2020, defined as a student remaining enrolled in at least one class past DTCC's census date. To test the efficacy of the treatment we report linear probability or hierarchical linear models utilizing intent-to-treat estimates in which all students in the treatment condition were included in the analyses, regardless of their engagement with the text-messaging platform. For our primary analyses, race categories were combined into one binary race variable (0 = White, 1 = student of color), due to the small numbers of students who identified as American Indian/Alaska Native, Asian2, Native Hawaiian/Pacific Islander, or Two or More Races. Predictors of enrollment included experimental condition, gender (0 = female, 1 = male), binary race, Spring 2020 enrollment, Summer 2020 enrollment, first generation status (0 = continuing generation, 1 = first-generation), and Pell eligibility (0 = ineligible, 1 = eligible). To better understand the impact of our treatment on equity, we also examined effects separately for Black/African American students, Hispanic/Latino students, and all other students of color. To examine heterogeneity of effects across individual characteristics, we then tested our treatment effect separately for student subgroups based on demographic factors for which we found a significant main effect. Finally, we examined heterogeneity of treatment effects based on student levels of engagement with the platform.
Results
Students' Engagement with Treatment
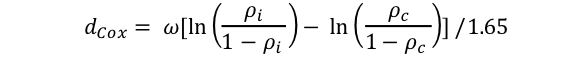
Table 2 displays the engagement of treatment students with messages. Because students with missing, incomplete, or invalid mobile numbers were excluded from the population prior to randomization, almost all students in the treatment group received the messages (98%). The remaining 2% had mobile numbers without service for the duration of the study. Only 4% of students unsubscribed from text messages on the first day after receiving the welcome message informing them that they could stop at any time; the cumulative percentage of students who unsubscribed over the summer was 11%. Students received an average of 17 messages, with the majority in question form (15, on average), and an observed maximum of 31 messages. Forty-one percent of treatment students responded at least once, with an average of just fewer than 3 replies per student. The most active student on the platform sent 20 replies.
We did not observe significant engagement differences between students who were enrolled in Spring 2020 and those who were not. Moreover, students enrolled in Summer 2020 concurrently with our study were equally likely to unsubscribe over the course of the summer as those who were not enrolled at the time (11% in each group). Students enrolled in Summer 2020, however, were significantly more likely than other students to respond at least once (45% vs. 38%), χ 2(1) = 6.62, p < 0.05. Men were more likely than women to unsubscribe on the first day (7% vs. 3%), χ2 (1) = 6.98, p < 0.05, but otherwise were equally likely to unsubscribe over the course of the summer and to respond at least once.
Compared to White students, students of color were less likely to unsubscribe over the course of the summer (8% vs. 15%), χ 2(1) = 18.88, p < 0.001, and more likely to respond at least once (49% vs. 34%), χ2(1) = 18.52, p < 0.001. Disaggregating these data revealed that Black/African American students were especially engaged, as they were most likely to respond at least once (51%) compared to White students (34%), χ2(1) = 28.93, p < 0.001, Hispanic/Latino students (39%), χ2(1) = 9.15, p < 0.01, and other students of color (41%), χ2(1) = 3.50, p = 0.06. Black/African American students were also less likely to unsubscribe both on the first day (2% vs. 5%), χ 2(1) = 4.15, p < 0.05, and over the course of the summer (7% vs. 15%), χ2(1) = 17.10, p < 0.001, compared to White students. Hispanic/Latino students showed no other engagement differences compared to all other student groups. Other students of color were less likely than White students to unsubscribe over the course of the summer (7% vs. 15%), χ 2(1) = 5.95, p < 0.05, and trended toward a higher likelihood of responding at least once (41% vs. 34%), but this was not significant.
Table 2. Student Engagement with Text Messages
Treatment Effects
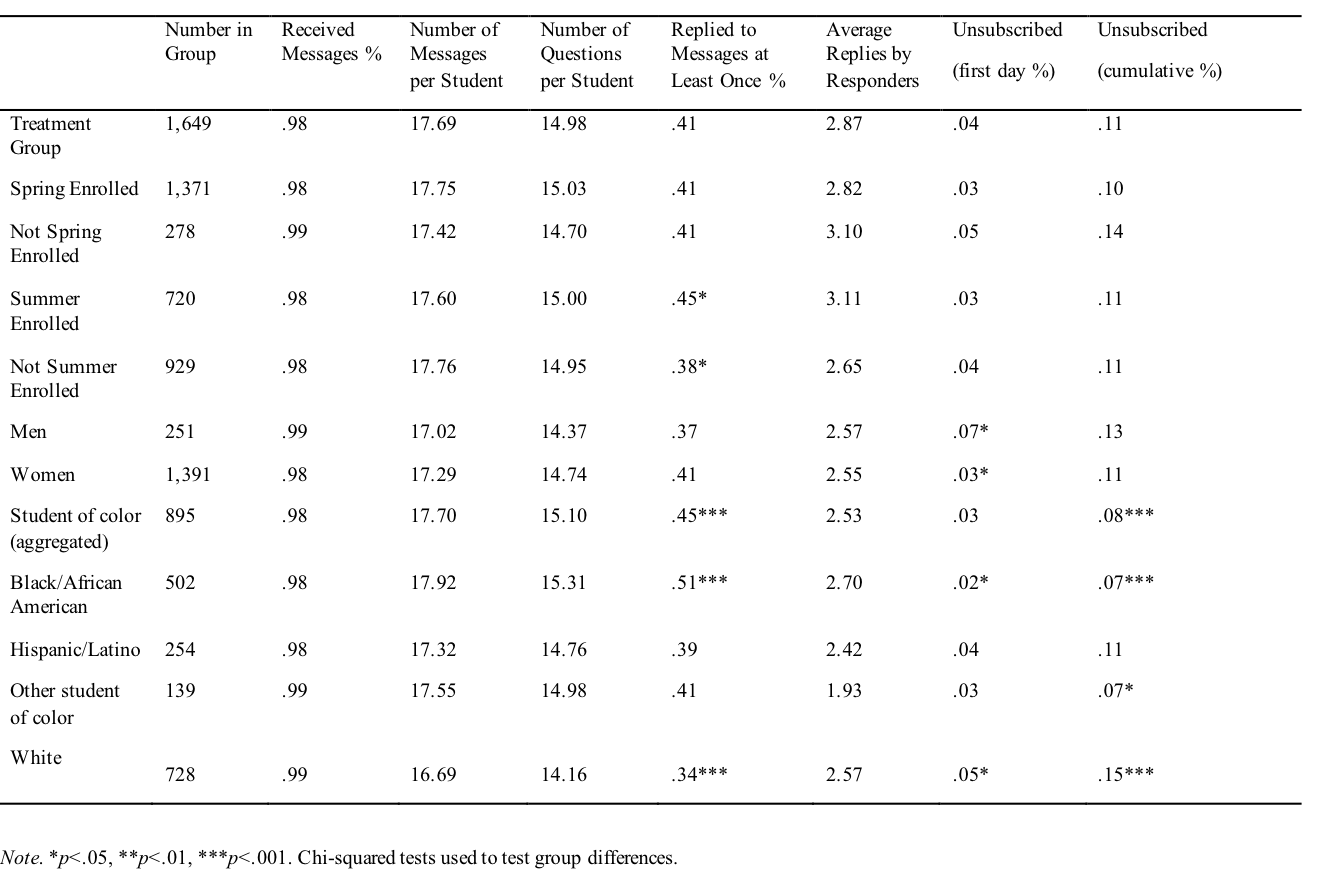
Linear probability models are presented in Table 3. We first examined the treatment effect (with significance and standard errors corrected in a hierarchical linear model with Spring 2020 enrollment entered as a random effect) and found that receiving messages improved Fall 2020 reenrollment by 3 percentage points compared to the control group rate of 71%. We also observed higher reenrollment among White students as compared to students of color (75% vs. 72%), women as compared to men (73% vs. 68%), and students enrolled in both the term prior to the study (Spring 2020; 76% vs. 61%), as well as the term concurrent to the study (Summer 2020; 88% vs. 62%). We next examined moderation by binary race, gender, spring enrollment, and summer enrollment. First-generation status and Pell eligibility were not significant predictors of Fall 2020 reenrollment for either the overall population or among any demographic subgroups, and were thus excluded from subsequent models.
In disaggregating the students of color variable, we found the same difference in Fall 2020 reenrollment of approximately 3 percentage points between White students and Black/African American students, Hispanic/Latino students, and other students of color, but these differences were not statistically significant due to the smaller sample sizes. Intergroup comparisons between Black/African American students, Hispanic/Latino students, and other students of color revealed no significant main effects predicting reenrollment. Because of the suggestive mean differences when comparing Black/African American, Hispanic/Latino, and other students of color with White students, and the academic inequities historically found based on race and ethnicity (Donini-Lenhoff & Brotherton, 2010; Pryjmachuk et al., 2009), we also examined moderation of the treatment effect separately for Black/African American students, Hispanic/Latino students, and all other students of color (each remaining racial category was too small to examine alone).
Table 3. Main Effects of Treatment and Individual Factors on Fall 2020 Reenrollment
Heterogeneity of Treatment Effects: Individual Differences
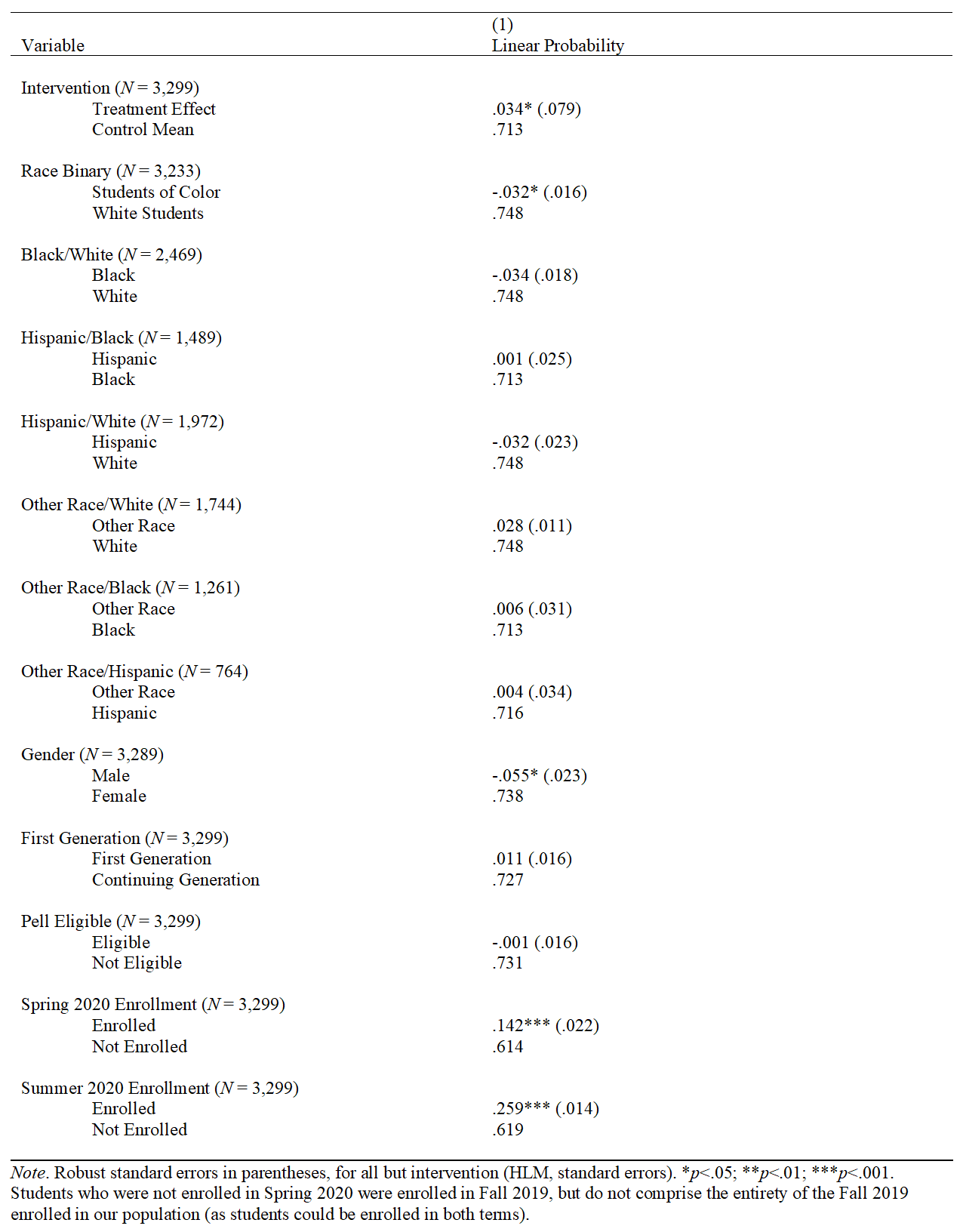
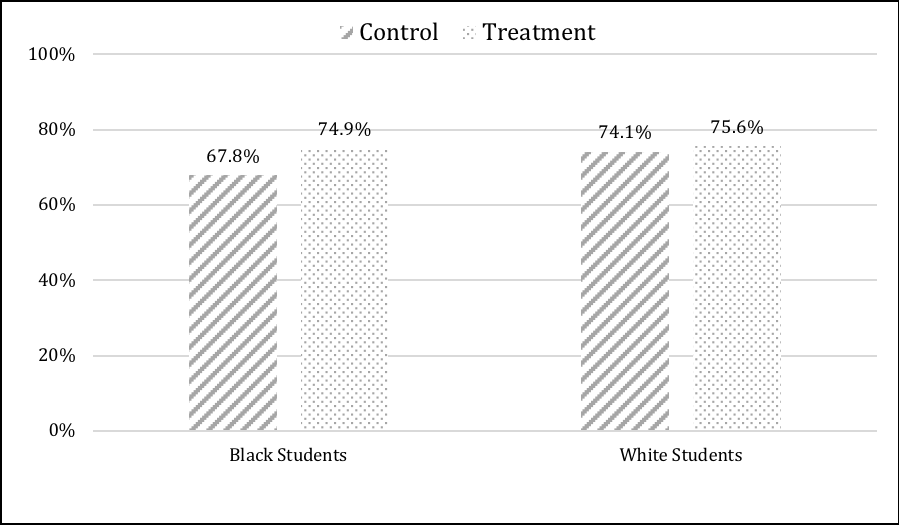
We next examined simple effects separately for each of the demographic variables for which we found significant (or nearly significant) impact on Fall 2020 reenrollment: gender, binary race, Black/African American students, Hispanic/Latino students, all other students of color, Spring 2020 enrollment, and Summer 2020 enrollment (see Table 4). As illustrated in Figure 1A, we found a significant effect for men, such that those who received treatment reenrolled at a rate 11 percentage points higher than the control group rate of 63%. Treatment did not have a significant impact for women, who reenrolled at a base rate of 73%. Our treatment, therefore, eliminated the expected gap in enrollment between men and women in this pre-allied health population (Pryjmachuk et al., 2009).
Table 4. Treatment Effects on Fall 2020 Reenrollment among Student Subgroups
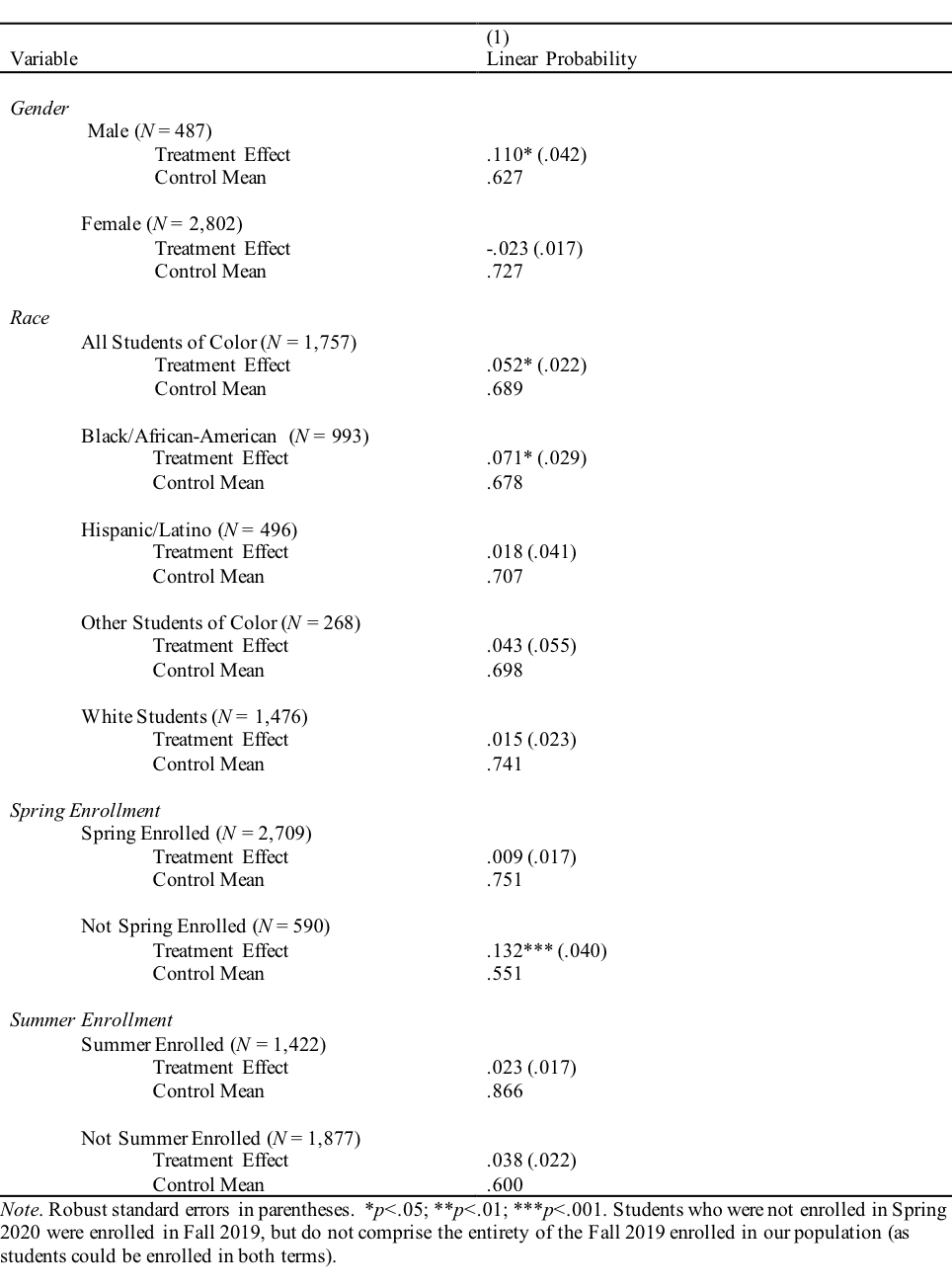
The treatment also disproportionately benefited all students of color when examined together, who reenrolled at a rate 5 percentage points higher than the control group rate of 68%. Disaggregating students of color, however, we found that the treatment primarily benefited Black/African American students who reenrolled at a rate 7 percentage points higher than the control group rate of 68% (see Figure 1B). Similar to the treatment effect for men, we eliminated the gap in Fall 2020 reenrollment between White and Black/African American students observed in the control condition, which reflected inequities in persistence seen historically (Donini-Lenhoff & Brotherton, 2010; Pryjmachuk et al., 2009). Other students of color in the treatment group reenrolled at a rate 4 percentage points higher than the control group rate of 70%, although this result was marginally significant owing to the smaller sample. White students and Hispanic/Latino students, however, showed no gains in reenrollment from treatment.
Finally, among students who were not enrolled in Spring 2020-but who had been enrolled in Fall 2019-those who experienced the treatment returned for Fall 2020 at a rate 13 percentage points higher than the control group rate of 55% (see Figure 1C). Although we observed a difference of nearly 4 percentage points in the hypothesized direction between treatment and control groups among students who were enrolled in Summer 2020, this difference failed to reach statistical significance.
Figure 1. Interactions between Experimental Condition and (A) Gender, (B) Race, and (C) Spring 2020 Enrollment on Fall 2020 Term Reenrollment
A
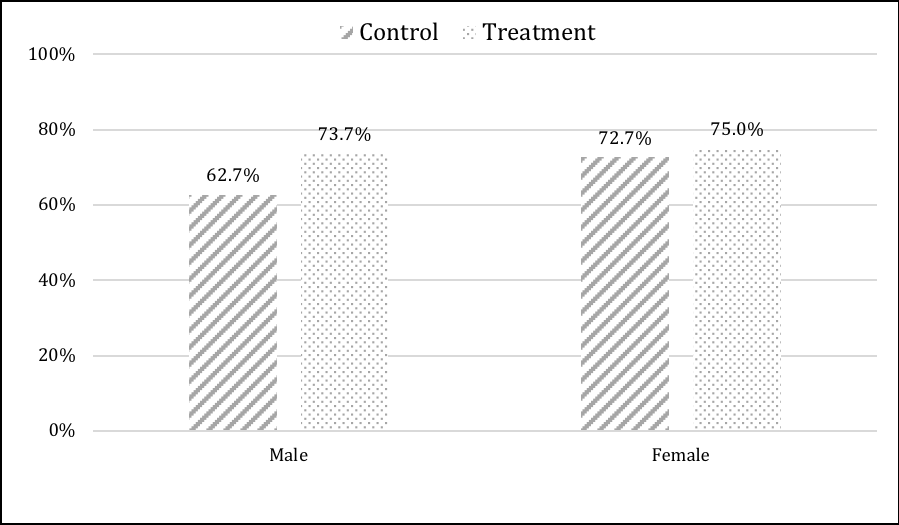
B
C
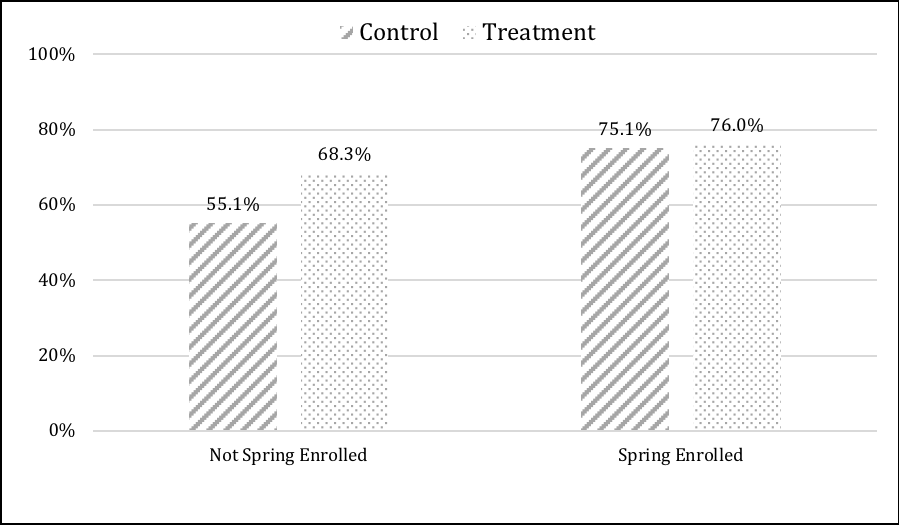
Note. Students who were not enrolled in Spring 2020 were enrolled in Fall 2019, but do not comprise the entirety of the Fall 2019 enrolled in our population (as students could be enrolled in both terms).
Heterogeneity of Treatment Effects: Student Engagement
To explore heterogeneity of effects based on student engagement, we divided treatment students into three groups based on the dose of treatment received (O'Hara & Sparrow, 2019): students who received no treatment (i.e., unsubscribed on the first day; n = 60), those who received partial treatment (i.e., students who received some messages but unsubscribed at some point during the study; n = 117), and those who received full treatment (i.e., students who remained subscribed for the duration of the study; n = 1,443). We further subdivided the full treatment group into those who never responded to a message (n = 809) and those students who responded at least once (n = 634). Because only 30 students unsubscribed after responding at least once, we did not subdivide those students in a similar fashion.
Students who received no treatment reenrolled for Fall 2020 at a rate 8 percentage points lower than the control group mean of 71%, although this finding lacked power to reach statistical significance. Reenrollment among students who received partial treatment (70%), as well those who received full treatment but did not respond (73%), did not significantly differ from the control group. Students who received the full treatment and responded at least once, however, enrolled at a rate 7 percentage points higher than the control group, t(2283) = 3.32, p < .001. These results dovetail with our findings on racial equity, in which Black/African American students were the most engaged with the platform and accrued the largest benefits in terms of Fall 2020 reenrollment.
Discussion and Implications
Our study adapted and combined three values-based interventions-values affirmation, goal congruence, and utility values-to support reenrollment among community college pre-allied health students, a key population for addressing growing workforce shortages in nursing and other skilled health professions (U.S. DHHS, 2017, 2019). We targeted students across Delaware's statewide community college system, and delivered our treatment via an interactive text-messaging platform, Persistence Plus. Overall, treated students reenrolled at higher rate than the control group, with those who had not been enrolled at DTCC in Spring 2020 more likely to return. Perhaps even more important, the treatment produced gains among men and Black/African American students, groups who face myriad barriers to entry, take longer to complete nursing and allied health programs, and are more likely to withdraw (Donini-Lenhoff & Brotherton, 2010; Hodges et al., 2017; Pryjmachuk et al., 2009).
Models of community college retention may provide a framework for understanding why these values-based interventions motivated students to persist. "Socio-academic integrative moments," for instance, have been identified as key to community college retention (Deil-Amen, 2011). These moments, which can occur between students and faculty, staff, or peers, and either in or out of the classroom, boost students' perceptions of warmth, supportiveness, and approachability attributed to their college; enhance their sense of belonging, identity, and competence; and improve their strategies around goal attainment. Although conceptualized as moments that occur interpersonally, our treatment may have reproduced elements of socio-academic integration digitally, which may be especially useful in the context of online learning. The proactive nature of the treatment, as well, may have increased impact by reducing the burden on students to self-identify a need for help and providing immediate response (Chan et al., 2019).
Finally, the impact of such interventions may be especially great for underrepresented students who perceive them as providing "validation" (Rendón, 1994). Retention of underrepresented students often requires validating interpersonal experiences that quell their self-doubt; again, these exercises may have reproduced elements of validation digitally during a period of physical disconnect from faculty, advisors, and peers. Although the absence of effects for Hispanic/Latino and other students of color could be attributed to insufficient power, the different engagement patterns and outcomes amongst these groups raise questions about whether values-based interventions must be culturally appropriate. Future research should explore the impact of tailoring these kinds of interventions to student groups beyond blanket categories such as students of color or first-generation.
Using Values-based Interventions to Address Healthcare Labor Shortages
Community colleges have a pivotal role to play in public health by addressing growing shortages of nursing and other healthcare professionals (Falatah, 2021; Willgerodt et al., 2018; Xu et al., 2020). Moreover, colleges' retention practices impact equity within the healthcare field. Increasing skills and opportunities for people of color not only provides a path out of the lowest-paying healthcare professions (Snyder et al., 2015), but may also benefit communities of color by reducing healthcare discrimination and improving public health (Phillips & Malone, 2014; Wilbur et al., 2020). Moreover, better support for men, who face numerous barriers to entry into nursing and allied health professions (Hodges et al., 2017), will help to further reduce workforce gaps. Community college leaders should, therefore, consider values-based interventions in their enrollment, retention, and equity strategies. Although the utility of these exercises as in-class or online assignments is clear (e.g., Harackiewicz et al., 2014; Miyake et al., 2010), our research suggests digital media, such as texting, may be a more scalable and engaging way to deliver these interventions (O'Hara & Sparrow, 2019). Moreover, digital media provide more flexibility to customize messages based on student data and responses.
Our results also indicate that values-based interventions benefit students who have stopped out of college, not just those currently enrolled. Although most prior studies of text message interventions have targeted college-intending high school seniors or currently enrolled college students (e.g., Castleman & Page, 2015, 2016; O'Hara & Sparrow, 2019; Page & Gehlbach, 2017; see Ortagus et al., 2021, for an exception), we found that our treatment increased reenrollment by 13 percentage points when students had stopped out prior, as opposed to only 4 percentage points when they had been recently enrolled. As community college enrollments have fallen almost 15% since the onset of the COVID-19 pandemic (National Student Clearinghouse, 2021), severely undercutting tuition revenue and keeping colleges understaffed, boosting enrollments back to pre-pandemic levels may be key to ensuring continued student success. Moreover, reenrolling students with prior credits ("comebackers"; Sheffer et al., 2020) is perhaps the most efficient way to improve individuals' economic prospects and fill vacant healthcare positions.
Contributions to Research on Values-based Interventions
Values-based interventions have increased college students' interest in science, intentions to major in science and enter into a science career, and persistence in science pathways (e.g., Diekman et al., 2017; Harackiewicz et al., 2015; Hulleman et al., 2017; Miyake et al., 2010). However, evidence is limited whether these brief interventions work with students outside of traditional laboratory courses (i.e., biology and physics) and in community colleges. Previously, both a values affirmation and utility value intervention delivered to community college students produced mixed results (Canning et al., 2019; Tibbetts et al., 2018), suggesting that students may not face the same barriers at community colleges that they do at four-year institutions, such as stereotype threat and cultural mismatch (Steele, 1997; Stephens et al., 2012). Our results reaffirm evidence that these types of interventions can boost community college reenrollment (O'Hara & Sparrow, 2019). Future research should consider these kinds of psychosocial interventions within existing frameworks of community college retention, such as socio-academic integrative moments and validation theory (Deil-Amen, 2011; Rendón, 1994). Better synthesis of these literatures would provide numerous opportunities for learning, such as understanding when, why, and for whom values-based interventions improve outcomes, and designing new ways to foster validation and integration, even during challenging times such as a pandemic.
Our study also suggests a framework for scaling behavioral science interventions that does not sacrifice the personalization characteristic of successful, small-scale "nudging" (e.g., Castleman & Page, 2015, 2016; Page & Gehlbach, 2017). Recent attempts to scale nudge interventions nationwide have not significantly impacted student behavior (Avery et al., 2021; Bird et al., 2021). Several explanations have been offered as to why these efforts have not worked, including a reliance on one-way messaging (when hiring staff to reply to students is cost-prohibitive), a lack of personalized information, a lack of trust between the student and the sender, increased noise due to the proliferation of text-based campaigns and supports, and improved student services provided by high schools, colleges, and non-profit organizations that have closed the information and support gaps that these interventions once helped to fill (Castleman, 2021).
We contend that our "local" approach to scaling (Bird et al., 2021) addresses several of these challenges. First, partnering with an integrated, statewide community college system reduced heterogeneity in campus attributes and allied health program design, thereby allowing personalization of messages to both local context and student characteristics (e.g., program or major, enrollment status) without excessive burden placed on intervention designers or college staff. This approach also meant messages came from a trusted source, DTCC. Second, technology that parses student responses using natural language processing and appropriately replies reduces need for additional staff to manage a texting campaign, and can reduce burden on existing staff by automating the answering of students' basic informational questions. Finally, there is no changing the fact that students receive more text messages than ever before. We believe, however, that interactive, supportive, and evidence-based messages are welcomed by students in need of extra encouragement, especially during the COVID-19 pandemic, given the positive feedback that several students texted to us at the end of the study. To share one such sentiment, "thank you so much!! the del tech support is always available, prompt with responses, very helpful, and alleviates the anxieties i have if i need a question answered immediately. thank you guys for all that you do! ©".
Limitations and Future Research
Several limitations to this research are worth noting. First, we only measured reenrollment past the DTCC census date for Fall 2020, mere weeks after the end of treatment. Although values affirmation and utility value interventions have produced significant impacts months to years later (Hecht et al., 2019; Layous et al., 2017; Tibbetts et al., 2016), we do not yet know whether text-based interventions produce similarly long-lasting effects, nor whether effects last among our community college and allied health populations. Second, we were unable to confirm whether reenrolled participants continued on the allied health track. Although increasing reenrollment is a win for both students and DTCC, keeping students motivated to enter into healthcare professions is necessary for addressing the aforementioned labor and equity gaps. Third, our control group received business as usual support from DTCC. A more stringent test would compare our treatment to a placebo-like text message program, perhaps comprised of one-way informational messages. Likewise, our treatment combined three different values-based interventions with messages about registration and student resources. Given our omnibus approach, we cannot determine whether these components had additive effects, synergistic effects, or whether some had no effect at all. Future experiments could isolate the various components to determine the efficacy of translating these values-based interventions to text messages, as well as measure theoretically meaningful mediators, such as college belonging, identity, and competence (Deil-Amen, 2011). Finally, our experiment conceptually replicated an earlier STEM intervention (O'Hara & Sparrow, 2019), but with a few key differences in results: a larger impact of the intervention on students who had stopped out, as opposed to concurrently enrolled students, and impact only for students who responded to the messages, as opposed to all treated students. Given that applying values-based interventions to community college populations is in its nascent stages, other researchers should test these strategies with other student groups to understand the relevant boundary conditions for when, where, and for whom these interventions improve academic persistence and performance.
Conclusion
New approaches to enrollment and retention within nursing and allied health programs are needed to address significant and growing workforce shortages, as well as equity gaps. Values-based interventions delivered via interactive text messages improved persistence among community college pre-allied health students. Effects were strongest amongst underrepresented students (men and Black/African American students) and when students had not been enrolled the semester prior to treatment. These behavioral science strategies should be employed by community college practitioners to improve persistence among their nursing and allied health students, remedy healthcare workforce needs, and increase educational and professional equity within these fields.
Acknowledgments
Our thanks go to Melissa Rakes and Amber King at Delaware Technical Community College for their help with study design and implementation, and to the rest of the team at Persistence Plus for their essential contributions.
Footnote
1DTCC programs in allied health are dental hygiene, diagnostic medical sonography, emergency medical technician (EMT), histotechnician, nuclear medicine technology, occupational therapy assistant, physical therapist assistant, radiologic technology, respiratory care technology, surgical technology, and veterinary technology.
2Although Asian students face prejudice and discrimination, especially during the COVID-19 pandemic, historically they exhibit the lowest attrition rates in allied health of any group (Donini-Lenhoff & Brotherton, 2010). We tested the treatment effect with Asian students removed from the aggregated students of color variable, and the results remained largely unchanged.References
Abdalla, M., Chiuzan, C., Shang, Y., Ko, G., Diaz, F., Shaw, K….Shechter, A. (2021). Factors associated with insomnia symptoms in a longitudinal study among New York City healthcare workers during the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 18 (17), 8970. https://doi.org/10.3390/ijerph18178970
Avery, C., Castleman, B. L., Hurwitz, M., Long, B. T., & Page, L. C. (2021). Digital messaging to improve college enrollment and success. Economics of Education Review, 84, 102-170. https://doi.org/10.1016/j.econedurev.2021.102170
Bird, K. A., Castleman, B. L., Denning, J. T., Goodman, J., Lamberton, C., & Rosinger, K. O. (2021). Nudging at scale: Experimental evidence from FAFSA completion campaigns. Journal of Economic Behavior & Organization, 183, 105-128. https://doi.org/10.1016/j.jebo.2020.12.022
Boyle, P. (2021, September 7). Hospitals innovate amid dire nursing shortages. Association of American Medical Colleges. https://www.aamc.org/news-insights/hospitals-innovate-amid-dire-nursing-shortages
Brown, E. R., Smith, J. L., Thoman, D. B., Allen, J. M., & Muragishi, G. (2015). From bench to bedside: A community utility value intervention to enhance students' biomedical science motivation. Journal of Educational Psychology, 107(4), 1116-1135. https://doi.org/10.1037/edu0000033
Bureau of Labor Statistics, U.S. Department of Labor.Occupational Outlook Handbook. (Sept 8, 2021). Healthcare occupations. https://www.bls.gov/ooh/healthcare/home.htm#:~:text=Employment%20in%20healthcare%20occupations%20is,of%20the%20other%20occupational%20groups
Bureau of Labor Statistics, U.S. Department of Labor, The Economics Daily. (May 6, 2019). Occupational requirements and benefits for nurses in the United States in 2018 . https://www.bls.gov/opub/ted/2019/occupational-requirements-and-benefits-for-nurses-in-the-united-states-in-2018.htm
Cai, Q., Feng, H., Huang, J., Wang, M., Wang, Q.…Liu, Y. (2020). The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: A case-control study. Journal of Affective Disorders, 275, 210-215. https://doi.org/10.1016/j.jad.2020.06.031
Canning, E. A., Harackiewicz, J. M., Priniski, S. J., Hecht, C. A., Tibbetts, Y., & Hyde, J. S. (2018). Improving performance and retention in introductory biology with a utility-value intervention. Journal of Educational Psychology, 110(6), 834-849. https://doi.org/10.1037/edu0000244
Canning, E. A., Priniski, S. J., & Harackiewicz, J. M. (2019). Unintended consequences of framing a utility-value intervention in two-year colleges. Learning and Instruction, 62, 37-48. https://doi.org/10.1016/j.learninstruc.2019.05.001
Castleman, B. L. (May 3, 2021). Why aren't text message interventions designed to boost college success working at scale? Behavioral Scientist. https://behavioralscientist.org/why-arent-text-message-interventions-designed-to-boost-college-success-working-at-scale/
Castleman, B. L., & Page, L. C. (2016). Freshman year financial aid nudges: An experiment to increase FAFSA renewal and college persistence. Journal of Human Resources, 51(2), 389-415. https://doi.org/10.3368/jhr.51.2.0614-6458R
Castleman, B. L., & Page, L. C. (2015). Summer nudging: Can personalized text messages and peer mentor outreach increase college going among low-income high school graduates? Journal of Economic Behavior & Organization, 115, 144-160. https://doi.org/10.1016/j.jebo.2014.12.008
Chan, Z. C. Y., Cheng, W. Y., Fong, M. K., Fung, Y. S., Ki, Y. M.…Tsoi, W. F. (2019). Curriculum design and attrition among undergraduate nursing students: A systematic review. Nurse Education Today, 74, 41-53. https://doi.org/10.1016/j.nedt.2018.11.024
Davidson, P. M. (2020). Is nursing a STEM discipline - Does it matter and what can we do about it? Journal of Advanced Nursing, 76, 1-3. https://doi.org/10.1111/jan.14212
Deil-Amen, R. (2011). Socio-academic integrative moments: Rethinking academic and social integration among two-year college students in career-related programs. The Journal of Higher Education, 82(1), 54-91. https://doi.org/10.1080/00221546.2011.11779085
Diekman, A. B., Clark, E. K., Johnston, A. M., Brown, E. R., & Steinberg, M. (2011). Malleability in communal goals and beliefs influences attraction to STEM careers: Evidence for a goal congruity perspective. Journal of Personality and Social Psychology, 101(5), 902-918. https://doi.org/10.1037/a0025199
Diekman, A. B., Steinberg, M., Brown, E. R., Belanger, A. L., & Clark, E. K. (2017). A goal congruity model of role entry, engagement, and exit: Understanding communal goal processes in STEM gender gaps. Personality and Social Psychology Review, 21(2), 142-175. https://doi.org/10.1177/1088868316642141
Donini-Lenhoff, F. G., & Brotherton, S. E. (2010). Racial-ethnic diversity in allied health: The continuing challenge. Journal of Allied Health, 39(2), 104-109.
Falatah, R. (2021). The impact of the coronavirus disease (COVID-19) pandemic on nurses' turnover intention: An integrative review. Nursing Reports, 11(4), 787-810. https://doi.org/10.3390/nursrep11040075
Green, C., & John, L. (2020). Should nursing be considered a STEM profession? Nursing Forum, 55, 205-210. https://doi.org/10.1111/nuf.12417
Harackiewicz, J. M., Canning, E. A., Tibbetts, Y., Giffen, C. J., Blair, S. S., Rouse, D. I., & Hyde, J. S. (2014). Closing the social class achievement gap for first-generation students in undergraduate biology. Journal of Educational Psychology, 106(2), 375-389. https://doi.org/10.1037/a0034679
Harackiewicz, J. M., Canning, E. A., Tibbetts, Y., Priniski, S. J., & Hyde, J. S. (2015). Closing achievement gaps with a utility-value intervention: Disentangling race and social class.Journal of Personality and Social Psychology, 111(5), 745-765. https://doi.org/10.1037/pspp0000075
Harackiewicz, J. M., & Priniski, S. J. (2018). Improving student outcomes in higher education: The science of targeted intervention. Annual Review of Psychology, 69, 409-435. https://doi.org/10.1146/annurev-psych-122216-011725
Harris, R. C., Rosenberg, L., & O'Rourke, M. E. G. (2014). Addressing the challenges of nursing student attrition. Journal of Nursing Education, 53(1), 31-37. https://doi.org/10.3928/01484834-20131218-03
Hecht, C. A., Harackiewicz, J. M., Priniski, S. J., Canning, E. A., Tibbetts, Y., & Hyde, J. S. (2019). Promoting persistence in the biological and medical sciences: An expectancy-value approach to intervention. Journal of Educational Psychology, 111(8), 1462-1477. https://doi.org/10.1037/edu0000356
Hodges, E. A., Rowsey, P. J., Gray, T. F., Kneipp, S. M., Giscombe, C. W., Foster, B. B….Kowlowitz, V. (2017). Bridging the gender divide: Facilitating the educational path for men in nursing. Journal of Nursing Education, 56(5), 295-299. https://doi.org/10.3928/01484834-20170421-08
Howell, J., Hurwitz, M., Ma, J., Pender, M., Perfetto, G., Wyatt, J., & Young, L. (2021). College enrollment and retention in the era of COVID. College Board. https://research.collegeboard.org/pdf/enrollment-retention-covid2020.pdf
Hu, D., Kong, Y., Li, W., Han, Q., Zhang, X.…Zhu, J. (2020). Frontline nurses' burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. EClinicalMedicine, 24, 100424. https://doi.org/10.1016/j.eclinm.2020.100424
Hulleman, C. S., Godes, O., Hendricks, B. L., & Harackiewicz, J. M. (2010). Enhancing interest and performance with a utility value intervention. Journal of Educational Psychology, 102(4), 880-895. https://doi.org/10.1037/a0019506
Hulleman, C. S., Kosovich, J. J., Barron, K. E., & Daniel, D. B. (2017). Making connections: Replicating and extending the utility value intervention in the classroom. Journal of Educational Psychology, 109(3), 387-404. https://psycnet.apa.org/doi/10.1037/edu0000146
Jordt, H., Eddy, S. L., Brazil, R., Lau, I., Mann, C., Brownell, S. E., King, K., & Freeman, S. (2017). Values affirmation intervention reduced achievement gap between underrepresented minority and white students in introductory biology classes. CBE-Life Sciences Education, 16(3), ar41. https://doi.org/10.1187/cbe.16-12-0351
Labrague, L. J., & de los Santos, J. A. A. (2020). COVID-19 anxiety among front-line nurses: Predictive role of organisational support, personal resilience and social support. Journal of Nursing Management, 28(7), 1653-1661. https://doi.org/10.1111/jonm.13121
Labrague, L. J., & de los Santos, J. A. A. (2021). Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. Journal of Nursing Management, 29(3), 395-403. https://doi.org/10.1111/jonm.13168
Layous, K., Davis, E. M., Garcia, J., Purdie-Vaughns, V., Cook, J. E., & Cohen, G. L. (2016). Feeling left out, but affirmed: Protecting against the negative effects of low belonging in college. Journal of Experimental Social Psychology, 69, 227-231. https://doi.org/10.1016/j.jesp.2016.09.008
Loughran, T. J., Harpel, T., Vollmer, R., & Schumacher, J. (2018). Effectiveness of intuitive eating intervention through text messaging among college students. College Student Journal, 52(2), 232-244.
Miyake, A., Kost-Smith, L. E., Finkelstein, N. D., Pollock, S. J., Cohen, G. L., & Ito, T. A. (2010). Reducing the gender achievement gap in college science: A classroom study of values affirmation. Science, 330, 1234-1237. https://doi.org/10.1126/science.1195996
National Student Clearinghouse. (2021, November 18). Stay informed with the latest enrollment information. National Student Clearinghouse Research Center. https://nscresearchcenter.org/stay-informed/
O'Hara, R. E., & Sparrow, B. (2019). A summer nudge campaign to motivate community college STEM students to reenroll. AERA Open, 5 (3), 2332858419875715. https://doi.org/10.1177%2F2332858419875715
Ortagus, J. C., Tanner, M., & McFarlin, I. (2021). Can re-enrollment campaigns help dropouts return to college? Evidence from Florida community colleges. Educational Evaluation and Policy Analysis, 43(1), 154-171. https://doi.org/10.3102/0162373720979177
Page, L. C., & Gehlbach, H. (2017). How an artificially intelligent virtual assistant helps students navigate the road to college. AERA Open, 3(4), 2332858417749220. https://doi.org/10.1177/2332858417749220
Phillips, J. M., & Malone, B. (2014). Increasing racial/ethnic diversity in nursing to reduce health disparities and achieve health equity. Public Health Reports, 129(1.2, Suppl.), S45-50.
Prasad, K., McLoughlin, C., Stillman, M., Poplau, S., Goelz, E.…Sinsky, C. A. (2021). Prevalence and correlates of stress and burnout among U.S. healthcare workers during the COVID-19 pandemic: A national cross-sectional survey study. EClinicalMedicine, 35, 100879. https://doi.org/10.1016/j.eclinm.2021.100879
Pryjmachuk, S., Easton, K., & Littlewood, A. (2009). Nurse education: Factors associated with attrition. Journal of Advanced Nursing, 65 (1), 149-160. https://doi.org/10.1111/j.1365-2648.2008.04852.x
Reith, T. P. (2018). Burnout in United States healthcare professionals: A narrative review. Cureus, 10(12), e3681. https://doi.org/10.7759/cureus.3681
Rendón, L. I. (1994). Validating culturally diverse students : Toward a new model of learning and student development. Innovative Higher Education, 19(1), 33-51. https://doi.org/10.1007/BF01191156
Riley, W., Obermayer, J., & Jean-Mary, J. (2008). Internet and mobile phone text messaging intervention for college smokers. Journal of American College Health, 57(2), 245-248. https://doi.org/10.3200/JACH.57.2.245-248
Riordan, B., Flett, J. A. M., Conner, T. S., & Scarf, D. (2017). A text message intervention to reduce first year university students' alcohol use: A pilot experimental study. Digital Health, 3, 1-19. https://doi.org/10.1177/2055207617707627
Said, R. M., & El-Shafei, D. A. (2020). Occupational stress, job satisfaction, and intent to leave: Nurses working on front lines during COVID-19 pandemic in Zagazig City, Egypt.Environmental Science and Pollution Research, 28(7), 8791-8801. https://doi.org/10.1007/s11356-020-11235-8
Shechter, A., Diaz, F., Moise, N., Anstey, D. E., Ye, S.…Abdalla, M. (2020). Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. General Hospital Psychiatry, 66, 1-8. https://doi.org/10.1016/j.genhospsych.2020.06.007
Sheffer, H., Palmer, I., & Mattei, A. B. (2020). The comeback story: How adults return to school to complete their degrees. New America. https://www.newamerica.org/education-policy/reports/comeback-story/
Skillman, S. M., Keppel, G. A., Patterson, D. G., & Doescher, M. P. (2012). The contributions of community colleges to the education of allied health professionals in rural areas of the United States. Rural Health Research and Policy Centers.
Snyder, C. R., Stover, B., Skillman, S. M., & Frogner, B. K. (2015, July). Facilitating racial and ethnic diversity in the health workforce. Center for Health Workforce Studies. http://depts.washington.edu/uwrhrc/uploads/FINALREPORT_Facilitating%20Diversity%20in%20the%20Health%20Workforce_7.8.2015.pdf
Steele, C. M. (1997). A threat in the air: How stereotypes shape intellectual identity and performance. American Psychologist, 52(6), 613-629. https://doi.org/10.1037/0003-066X.52.6.613
Steinberg, M., & Diekman, A. B. (2018). Considering "why" to engage in STEM activities elevates communal content of STEM affordances. Journal of Experimental Social Psychology, 75, 107-114. https://doi.org/10.1016/j.jesp.2017.10.010
Stephens, N. M., Fryberg, S. A., Markus, H. R., Johnson, C. S., & Covarrubias, R. (2012). Unseen disadvantage: How American universities' focus on independence undermines the academic performance of first-generation college students. Journal of Personality and Social Psychology, 102(6), 1178-1197. https://doi.org/10.1037/a0027143
Tibbetts, Y., Harackiewicz, J. M., Canning, E. A., Boston, J. S., Priniski, S. J., & Hyde J. S. (2016). Affirming independence: Exploring mechanisms underlying a values affirmation intervention for first-generation students. Journal of Personality and Social Psychology 110(5), 635-659. https://doi.org/10.1037/pspa0000049
Tibbetts, Y., Priniski, S. J., Hecht, C. A., Borman, G. D., & Harackiewicz, J. M. (2018). Different institutions and different values: First-generation student fit at 2-year colleges. Frontiers in Psychology, 9, 502. https://doi.org/10.3389/fpsyg.2018.00502
U.S. Department of Health and Human Services, Health Resources and Services Administration, National Center for Workforce Analysis. (2019). Brief summary results from the 2018 National Sample Survey of Registered Nurses . https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/nssrn-summary-report.pdf
U.S. Department of Health and Human Services, Health Resources and Services Administration, National Center for Workforce Analysis. (2017). National and regional supply and demand projections of the nursing workforce: 2014-2030 . https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/nchwa-hrsa-nursing-report.pdf
Weissman, S. (2021, November 4). Struggling to fill a dangerous and growing labor gap. Inside Higher Ed. https://www.insidehighered.com/news/2021/11/04/colleges-and-universities-strive-graduate-more-nurses
What Works Clearinghouse. (2020). Standards handbook (v.4.1). Washington, DC: U.S. Department of Education, Institute of Education Sciences, National Center for Education Evaluation and Regional Assistance. https://ies.ed.gov/ncee/wwc/Docs/referenceresources/WWC-Standards-Handbook-v4-1-508.pdf
Wilbur, K., Snyder, C., Essary, A. C., Reddy, S., Will, K. K., & Saxon, M. (2020). Developing workforce diversity in the health professions: A social justice perspective. Health Professions Education, 6(2), 222-229. https://doi.org/10.1016/j.hpe.2020.01.002
Willgerodt, M. A., Brock, D. M., & Maughan, E. D. (2018). Public school nursing practice in the United States. The Journal of School Nursing, 34(3), 232-244. https://doi.org/10.1177/1059840517752456
Xu, H., Intrator, O., & Bowblis, J. R. (2020). Shortages of staff in nursing homes during the COVID-19 pandemic: What are the driving factors? Journal of the American Medical Directors Association, 21(10), 1371-1377. https://doi.org/10.1016/j.jamda.2020.08.002
Zangaro, G. A., Streeter, R., & Li, T. (2018). Trends in racial and ethnic demographics of the nursing workforce: 2000 to 2015. Nursing Outlook, 66(4), 365-371. https://doi.org/10.1016/j.outlook.2018.05.001
Appendix: Sample Messages by Values-Based Intervention
Values Affirmation
Reaffirming important values can reduce stress during hard times. Which of these is most important to you? Text: Kindness, Curiosity, Ambition, Friendship
[RESPONSE: Kindness] How does being kind relate to studying health at DTCC? Write a few sentences about how kindness defines your education & future goals.
Goal Congruence
Which of these would most excite you about working in a health career? Text: Helping people, working in community, being part of team, contributing to society
[RESPONSE: Helping people] We need skilled & passionate health care workers now more than ever. If you hit a rough patch just remember how many lives you'll better in your career.
Utility value
Studying health has benefits right away, not just in your future career. [STUDENT_FIRSTNAME], what's 1 thing you've learned at DTCC that's been helpful this summer?
[RESPONSE: Open-ended] College can focus a lot on career readiness but the lessons you learn can be useful today. Reflect on these opportunities to help you stay focused in school.
*Contact: ross@persistenceplusnetwork.comJournal of Postsecondary Student Success, Volume 1, Issue 3